Health is really all a question of balance. Not too much of this, not too little of that. Gout is no exception. Throughout history, this particular form of arthrosis has been associated with the exaggerated consumption of rich foods and excessive alcohol, and consequently described as "arthritis of the rich" since, in the early days, only the higher classes of society seemed to suffer from it. However, as the excessive indulgence in over-rich foods has spread across a great part of the world, gout too has spread - and not only on a geographical scale but also throughout the various strata of human society. Gout is an inflammation caused by the accumulation of needle-like crystals of uric acid deposited in joints, tendons or their surrounding tissues. Uric acid comes from the breakdown of purine we ingest from the food we eat, and is usually processed by our kidneys and then eliminated with our urine. When too much uric acid is produced however, it precipitates as urate crystals that slowly build up finally causing excruciating pain - surprisingly at the base of the big toe in about half of gout cases. Why is uric acid elimination sometimes insufficient? Besides certain diets, there are a number of other reasons and one of them is the inherited dysfunction of a protein pump known as ABCG2.
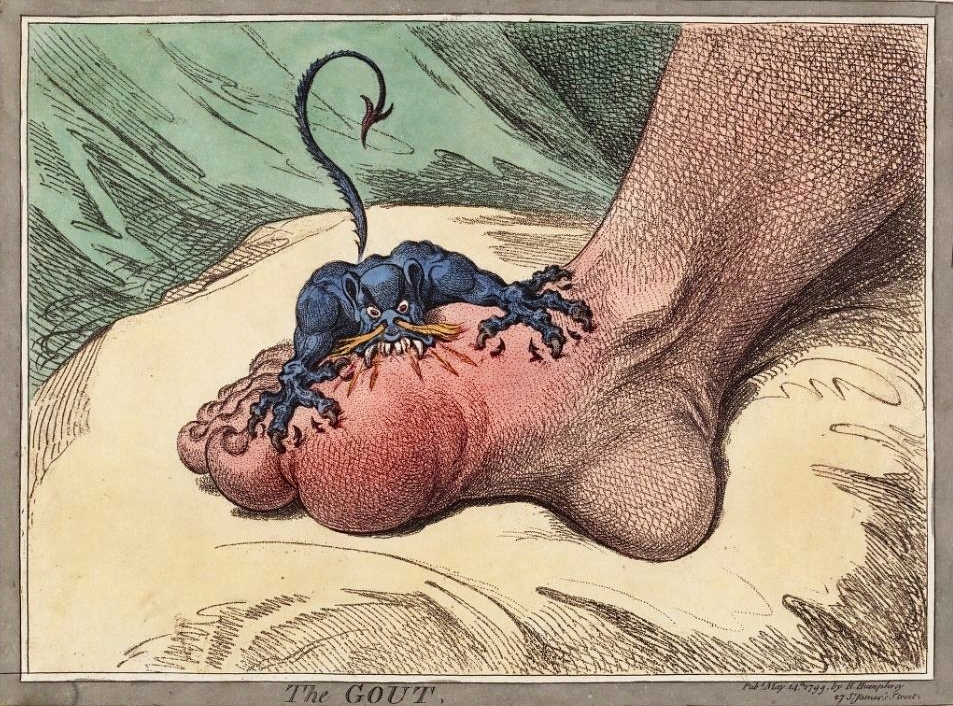
The Egyptians gave the first written account of gout - gout of the toe, or podagra - over 2,500 years ago, making it one of the oldest diseases in history. Hippocrates called it the "unwalkable disease" since the pain was so acute, those suffering from it were unable to walk. Centuries later, the English physician Thomas Sydenham was to talk of podagra as "[...] so exquisitely painful as not to endure the weight of the clothes nor the shaking of the room from a person walking briskly therein." Hippocrates had noted the link between gout and those who indulged in too many rich foods and alcohol, and half a century later, Galen associated the affliction with what he qualified as debauchery and intemperance - traits he stressed could also affect women since they "rival men in every kind of lasciviousness". The first to call the disease 'gout' - from the Latin 'gutta' meaning 'drop' - was the Dominican monk Randolphus of Bocking in the 13th century when scholars still believed that health and temperament depended on a balance between four main bodily fluids or humors. Gout was simply the result of one of the fluids dripping into our joints.
Thanks to the microscope, in the 17th century Antonie van Leeuwenhoek was the first to distinguish and describe the presence of long transparent crystals in a gouty nodule. During the 19th century, their chemical composition was identified as uric acid and their accumulation as the cause of inflammation. In the 1930s, scientists understood that gout can be inherited, and by the 1960s, uric acid was recognised as the end-product of purine metabolism. But where exactly do purines come from? Well, they exist bountifully in meat, seafood and beer for instance - which immediately highlights the diet problem in Western society. One astonishing observation: mammals have an enzyme that can break down uric acid. Yes, but all mammals save humans and apes. That is, we used to have it but Nature decided we would be better off without it. Why you may wonder. A possible answer: uric acid has an important anti-oxidant activity, and time did not bargain on us over-eating.
Source: Wikipedia
ABCG2 - or ATP-Binding Cassette, subfamily G, member 2, transporter - is a transporter with a surprisingly broad specificity. While many proteins deal with very few substrates if not only one, ABCG2 deals with as many as 200! Taking this into consideration, its involvement in purine metabolism may almost sound like an afterthought. Yet if it is dysfunctional, ABCG2 can bring about gout. How? ABCG2 is present in the small intestine and our kidneys where purine is broken down to uric acid. Here, ABCG2 participates in uric acid excretion by picking it up in the cytosol and driving it out of cells. When the protein is dysfunctional - as one of its inherited forms is - uric acid is not excreted and gradually piles up in the form of crystals, ultimately causing gout or indeed kidney stones. Here, gout is less a case of an overdose of purine than an innate metabolic deficiency.
How does ABCG2 actually excrete uric acid? It belongs to the very large family of ABC transporters that are vital for an organism's first line of defence against toxins - and one of the many transporters that give chemotherapy a tough time because they also see therapeutic drugs as undesired entities and dutifully force them out of malignant cells. ABCG2 has therefore become an important therapeutic target and been extensively studied. The protein is transmembrane and has a small nucleotide-binding domain (NBD) that dangles into the cytosol from one extremity. Two ABCG2 monomers, at least, are necessary for the transporter to function properly. During purine metabolism, uric acid binds to the transmembrane region of ABCG2. ATP subsequently binds to the NBD region causing it to tighten and rotate by about 35 degrees. This rotation twists the transmembrane region in such a way that the substrate is literally squeezed into the extracellular medium. ATP hydrolysis follows causing ABCG2 to spring back to its more relaxed posture, ready to pick up some more uric acid .
Up until the 19th century, the most popular remedy for gout was the purgative colchicine, an alkaloid from the autumn crocus Colchicum autumnale. However, the more we discover about gout and purine metabolism, the more we refine therapies and, today, choice drugs against gout are anti-inflammatory. Besides a change in diet, allopurinol is the most popular therapy offered as it interferes with the purine pathway by inhibiting the synthesis of uric acid altogether. However, with ABCG2's increasing popularity, the knowledge of its 3D structure is making it an ideal therapeutic candidate. Its activity could be modulated for those gout patients, for instance, who do not respond to allopurinol. It could also be engineered to control the level and location of its expression so as not to interfere with a patient undergoing chemotherapy for instance. This said, though proteins such as ABCG2 may sound like a panacea, the simple fact that they are involved in so many different tasks means that any change made to them is liable to affect more than just one metabolic pathway in a cell, thus perhaps raising more problems than offering solutions.

